
Here are the top stories recently covered by DocWire News in the hematology/oncology section. In this edition, read about cancer treatment and fertility in young women, shortened survival times in colorectal cancer due to COVID-19, a combination treatment for pancreatic cancer, osteopathic medicine for chemotherapy side effects in pediatric oncology, and more.
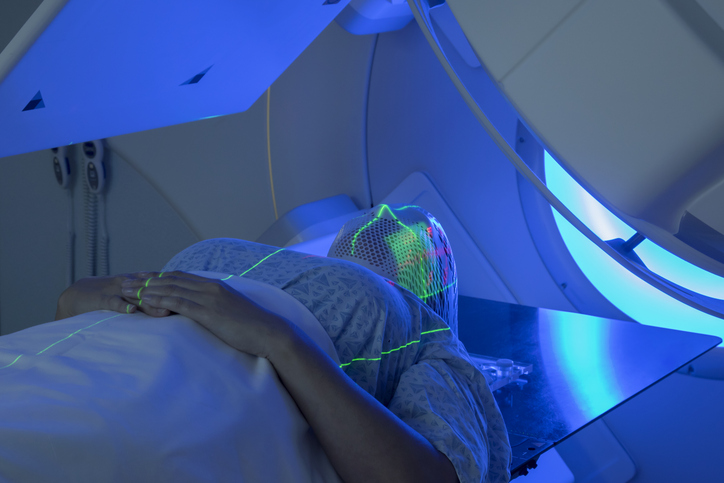
Cancer treatment does not end fertility in young women, according to the findings of a study that was presented at 36th Annual Meeting of ESHRE. In this study, researchers assessed data on 879 young female patients who were treated for a range of cancers between 2000 and 2019; all had sought counselling on preserving their fertility ahead of treatment. According to the results, the rate of those returning to make use of their frozen eggs and embryos is 16% (61/373), and 44 of them achieved a remarkably high birth rate of 71%, with a twin rate of 9%, when the fertilized eggs and embryos were transferred in an IVF procedure. Around two-thirds of patients returned within two years of their diagnosis; women with breast cancer were the most likely to return for fertility treatment. These patients also achieved the highest birth rates, significantly higher, for example, than those with lymphoma (70% vs 30%).
Surgical delays due to SARS-CoV-2 (COVID-19) are linked with shorter survival times in colorectal cancer, according to a new study. Following analysis, the results showed that a surgical delay of 30 to 40 days was correlated with shorter survival times in patients with colon cancer, as was a delay of seven to eight weeks after chemotherapy and/or radiation therapy in patients with rectal cancer. For pancreatic cancer, the investigators identified nine studies, and observed in two studies that cancer progression increased in patients who experienced surgical delays over 30 days. Moreover, six studies were included for gastric cancer, and none of the studies found worse patient survival outcomes with surgery delays.
A phase I/II study examined treatment strategies for patients with pancreatic cancer and peritoneal metastasis. After assessing a combination of intravenous gemcitabine, intravenous nab‐paclitaxel, and intraperitoneal paclitaxel, the study authors concluded, “Adding intraperitoneal paclitaxel had clinical efficacy with acceptable tolerability,” and plans for a phase III trial are now underway. The researchers assessed the frequencies of dose-limiting toxicities, with the recommended dose being established in phase I. Phase II focused on the one-year overall survival rate, with other outcomes including antitumor effects, symptom-reliving effects, safety, and overall survival. Per the phase I results, the recommended dose of intravenous gemcitabine was 800 mg/m2, of intravenous nab-paclitaxel was 75 mg/m2, and of intraperitoneal paclitaxel was 20 mg/m2. A total of 46 patients were enrolled in phase II. The median (range) time to treatment failure was six (zero to 22.6) months. The response rate was 21 of 43, and the disease control rate was 41 of 43. Among 30 total patients, ascites disappeared in 12; among 46 total patients, cytology became negative in 12. Median survival was 14.5 months. One-year overall survival rate was 61%. Eight patients of the total cohort underwent conversion surgery; patients who underwent resection had a significantly longer survival time than those who did not undergo surgery (median survival not reached vs. 12.4 months). Thirty-five patients in the total cohort sustained grade 3 to 4 hematological toxicities, and seven patients sustained non-hematological adverse events.
The use of osteopathic medicine in young cancer patients receiving chemotherapy was the subject of a recent study. Chemotherapy causes significant side effects in pediatric cancer patients—including pain, nausea, fatigue, psychosocial effects, and more—raising concerns among their caregivers and clinicians. There are some strategies to treat these episodes, but those often come with unpleasant effects of their own. Supportive care therapies including physical therapy, complementary and alternative medicine, and massage therapy have all been tried as add-ons to pharmacologic therapies, with mixed results. Viable options are needed to prevent these side effects as well as control their symptoms. What about osteopathic medicine? According to the researchers, there are significant knowledge gaps regarding osteopathic medicine among clinicians, caregivers, and patients; however, many of them are open to the idea.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.