
Here are the top stories recently covered by DocWire News in the hematology/oncology section. In this edition, read about mortality in one- versus five-star hospitals, the needs of bereaved cancer caregivers, the role of human papilloma viruses in prostate cancer, and long-term effects of a new radiotherapy does in breast cancer.
A new study finds that one-star hospitals have markedly higher rates of mortality in complex cancer surgeries juxtaposed hospitals with a five-star rating. Researchers evaluated the Center for Medicare and Medicaid Services’ “Star Rating” system, which is based on 62 measurements (e.g. mortality, readmissions, patient experience), but is not specific to any medical operation or patient population. They assessed 105,823 patients (65 years and older) who underwent complex cancer procedures at 3,146 hospitals between 2013 and 2016. The results showed the mortality rate over a 90-day period was associated with the star system, with the greatest difference observed between the 1-star (10.4%) and 5-star (6.4%) hospitals. However, these rates varied by surgery type.
Acting as a caregiver for a patient with cancer can take a significant toll, especially when the caregiver is the patient’s spouse. A study took a closer look at the psychosocial wellbeing of spousal caregivers who lose their partners to cancer at an older age. The researchers found that having a social support network can be beneficial for bereaved caregivers—putting nurses in a prime position to help during this difficult part of life.
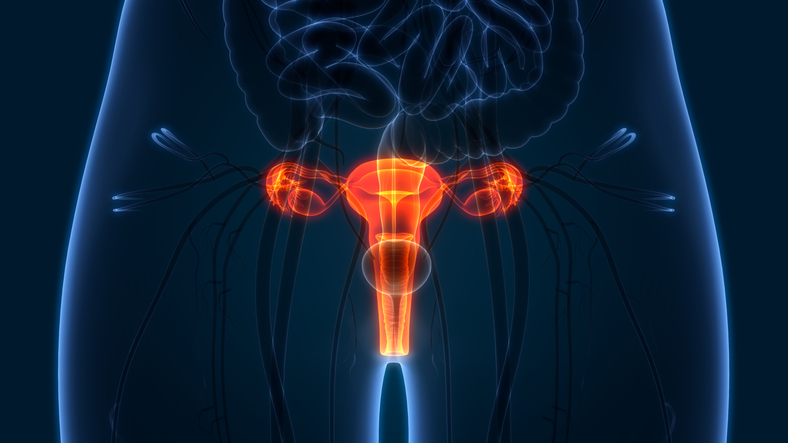
Human papilloma viruses (HPVs), a common group of viruses known to cause cervical cancers, may also play a role in prostate cancer. According to the results of a study, high-risk HPV types 16 and 18, which cause most cervical cancers, have been identified in normal, benign and malignant prostate tissues. The researchers observed in several case control studies, the prevalence of high-risk HPV DNA, which indicates the presence of cancer-causing types, was notably higher in prostate cancers juxtaposed to normal and benign prostate controls. The results showed in recent studies that 231 of 1071 prostate cancers (21.6%) were HPV positive, whereas only 74 of 1,103 benign prostate patients, only 6.7% were HPV positive.
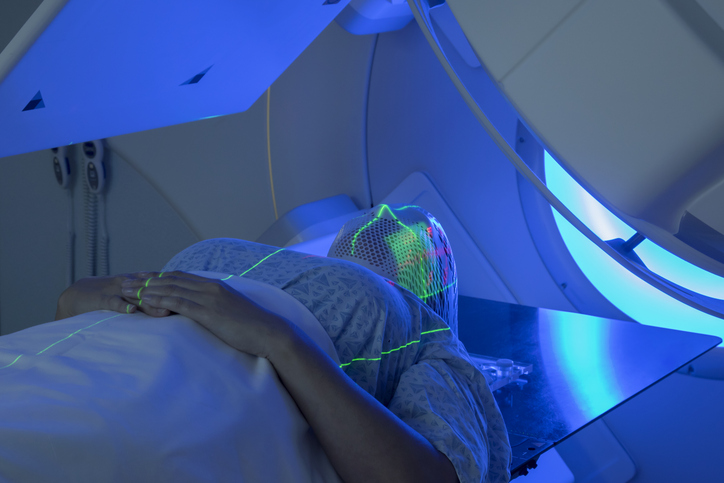
A 10-year study found that breast cancer patients receiving radiotherapy may have similar outcomes and side effects if they receive a few large doses of radiotherapy or a higher number of smaller doses, even if the former adds up to a lower total amount. The study may be promising for patients who cannot tolerate the side effects associated with daily radiation treatment.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.