
According to new information published in the Time from the U.S. Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee virtual meeting on April 6, the current COVID-19 booster strategy isn’t sustainable in the long-term. The committee reviewed vaccine effectiveness data to come up with better strategies for minimizing the virus.
Because the Centers for Disease Control (CDC) and FDA are still learning exactly how COVID-19 works and what level of immunity is necessary, the current U.S. vaccination strategy consists of primary vaccinations followed by booster shots in an attempt to stop the virus in its tracks before the healthcare system is overwhelmed. This system is further complicated by a person’s current health status, age, and which vaccine they choose.
Currently, Pfizer-BioNTech mRNA is approved as the primary vaccine, with two doses for adults aged 16 and above with an additional booster for those aged 12 and up. It’s also been authorized for emergency use in patients aged 5-15, and the booster is only allowed in those aged 5-11 who have weak immune systems. The Moderna mRNA is another two-shot vaccine with a booster approved for those aged 18 and above, and Johnson & Johnsen-Janssen is a single-shot vaccine approved for those aged 18 and above with a booster shot. A second booster (fourth shot) was recently authorized for Pfizer and Moderna by the FDA for those above age 50 and immunocompromised patients.
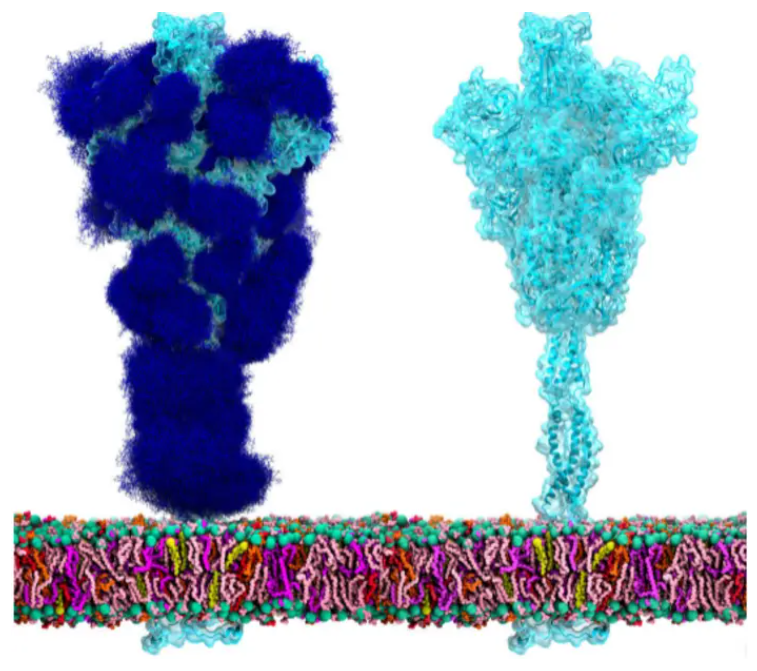
Seventy percent of eligible U.S. residents have received their primary shot, and 50 percent of that group has gotten their booster. However, according to a group of CDC scientists that spoke to the committee, the immunity provided by the vaccines and boosters weaken over time. The scientists said in studies where blood serum was taken from fully vaccinated participants and mixed with the Omicron variant, there was a 25-fold drop in neutralizing antibodies and for those who were boosted, only a 6-fold drop was found, proving a more effective method for curbing the virus is needed.
The committee discussed ways to better study vaccine effectiveness and come up with more sustainable options, including whether or when to change any primary vaccines or boosters. A flu shot-like model was discussed, but due to the lack of information about COVID-19’s genetic changes and unpredictability, this could be difficult. Whereas most flu shots are built the same, each COVID-19 shot has different makeup.
Lab-based studies like those that made the current authorizations and approvals possible were also discussed, where blood from fully vaccinated participants would be studied to see how well antibodies from the vaccines could neutralize the virus. A current study called COVAIL is looking at different primary and booster doses of both current and experimental vaccines targeting the original strain as well as the Omicron, Beta, and Delta variants.
Dr. Nadine Rouphael, who is professor of medicine and the executive director of the Hope Clinic at the Emory Vaccine Center, is co-chair of the COVAIL study and expects results early this summer. They say, “Could we come up with a strategy where we are not chasing variants but could make a vaccine that targets a cocktail of variants? The idea behind COVAIL is to take the available variant vaccines, either alone or in combination, and try to see how the immune responses they generate compare against the [original] vaccine.”






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.