A skills transfer course taking place at AAO 2019 will focus on the diagnosis and treatment of diabetic retinopathy, including the role of pharmacotherapy. Data were collected from one study at three different timepoints evaluating the use of ranibizumab.
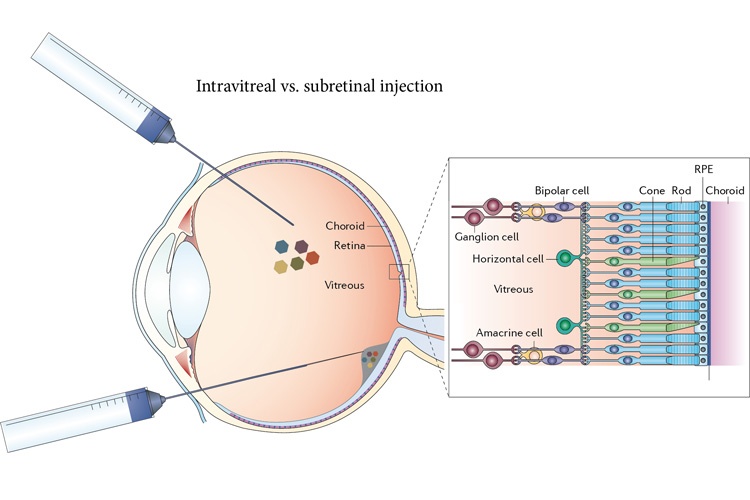
The first part of the study compared intravitreal 0.5 mg ranibizumab or 4 mg triamcinolone in combination with focal/grid laser compared to focal/grid laser treatment alone in diabetic macular edema. This trial randomized 854 study eyes (691 patients) to sham injection plus prompt laser (n = 293), 0.5 mg ranibizumab plus prompt laser (n = 187), 0.5 mg ranibizumab plus deferred (≥ 24 weeks) laser (n = 188), or 4 mg triamcinolone plus prompt laser (n = 186). The primary outcome was one-year best-corrected visual acuity and safety. After one year, the mean change in the visual acuity letter score from baseline was significantly greater in the ranibizumab plus prompt laser group (+9) and ranibizumab plus deferred laser group (+9) than the sham plus prompt laser group (+3), but the difference was not as significant in the triamcinolone plus prompt laser group (+4). Both ranibizumab groups and the triamcinolone group had greater reductions in mean central subfield thickness than the sham plus prompt laser group. The authors concluded that intravitreal ranibizumab with prompt or deferred laser was more effective for at least one year than prompt laser alone for the treatment of diabetic macular edema involving the central macula.
A three-year follow-up compared 361 patients randomized to ranibizumab every four weeks until visual acuity was no longer improving and prompt or deferred focal/grid laser treatment. The primary outcome was the same as the earlier report, but at three-year follow-up. The deferral group presented an estimated mean change in visual acuity letter greater than the prompt laser treatment group (9.7 letters vs. 6.8 letters; mean difference, 2.9 letters; 95% confidence interval, 0.4-5.4 letters; P = 0.02). In the deferral group, the percentage of eyes with a > 10-letter/gain loss was 56%, compared to 42% in the prompt group (P = 0.02); while the respective percentage of eyes with a > 10-letter gain/loss was 10% and 5% (P = 0.12). During the study period, the median number of injections in the prompt group was 12, compared to 15 in the deferral group (P = 0.007); at the three-year visit, the percentage of eyes with central subfield thickness ≥ 200 μm was 36% in both groups (P = 0.90). At this time, the authors concluded that there was no evidence to suggest that prompt focal/grid laser treatment was beneficial for vision outcomes in diabetic macular edema patients with fovea involvement; rather, the outcomes may be worse with prompt involvement.
At five-year follow-up, 124 patients in the prompt group and 111 in the deferred group were available for inclusion. The deferred group had a greater improvement in visual acuity letter score (+9.8 letters) than the prompt group (+7.2 letters; mean difference, -2.6 letters 95% CI, -5.5-+0.4 letters; P = 0.09). In the prompt versus deferred groups, the incidence of vision loss ≥ 10 letters was 46% and 58%, respectively, and improvement of ≥ 15 letters was 27% and 38%, respectively. During the five-year period, the median number of injections in the prompt group was 13, versus 17 in the deferral group; 54% and 45%, respectively, did not receive injections during year four, and 62% and 52%, respectively, did not receive injections during year five.
The researchers concluded their five-year outcomes report by stating that deferring laser treatment does not have significantly different outcomes compared to prompt treatment.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.