
Fractures related to osteoporosis may be costly among high-risk Medicare beneficiaries, according to recent research.
Researchers for the retrospective analysis evaluated information from the Health and Retirement Study (HRS). The study included Medicare claims data linked to HRS data for patients who were aged ≥ 65 years old, had at least one fracture risk factor, and had sustained a fracture between 1996 and 2008 (n = 689). Patients were propensity score-matched to 689 controls.
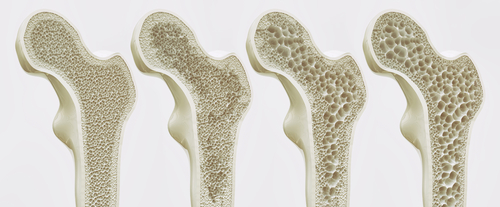
#MayoClinicMinute: Worldwide, 1 in 3 women over age 50 will experience a bone fracture due to #osteoporosis. But 1 in 5 men over age 50 also will have the same issue. https://t.co/uAUFLusTcT pic.twitter.com/lylTYbWAH1
— Mayo Clinic (@MayoClinic) October 10, 2018
Medicare expenditures for fracture cases increased by $13,929 (95% confidence interval [CI] = $11,920–15,938, P < 0.001) more when compared to the control group from the year before the fracture date to one year after the index date. The increase was most largely attributed to inpatient expenditures, which were $12,751 (95% CI = $10,790–14,7111, P < 0.001) more for fracture cases. Growth costs did not greatly differ two and three years post-fracture. Researchers observed no differences based on fracture location (hip or other site).
https://twitter.com/McGowanSpinal/status/1050144424574013440
Kandice A. Kapinos, PhD, a professor, health and labor economist at the RAND Corporation, and lead study author, said in an interview with MedicalResearch.com that the study’s greatest takeaway is, “Most of the large healthcare costs associated with osteoporotic fractures are incurred within the first year of a fracture and do not persist beyond that among older adults residing in community-based settings.”
New work with @shirafischer on the longer-term medical costs of #fractures among high-risk #Medicare beneficiaries. Summary @medresearchnews: https://t.co/fHI9qTx2g6
Link to paper: https://t.co/W83tAPVbqi
— Kandice Kapinos (@kandicekapinos) October 8, 2018
However, Kapinos also said that fracture patients likely incur additional medical costs after fracture not captured by the study.
“Despite there not being longer-term increases in direct healthcare costs for those with fractures, we found in related research that fractures are associated with limitations of functional health, including limitations to activities of daily living, mobility, and gross and fine motor skills up to four years after a fracture, though the effects do diminish over time,” Kapinos said. “Thus, these limitations may impose other longer-term financial costs that are not quantified in our current study. Future research could examine some of these other costs that are not direct healthcare costs.”
Health Care Costs Associated With Osteoporotic Fractures – @kandicekapinos discusses our recent paper https://t.co/rZsoGlbclY
— Shira Fischer (@shirafischer) October 10, 2018
The study authors collectively concluded: “Costs may be greater for those in skilled nursing and similar facilities and for those who have had a previous fracture.” Inflammation and Bone Density in Older Adults: What’s The Relationship? Zoledronate Effective in Fracture Protection for Women with Osteopenia Large Study Links Diabetes to OA, OP, and RA
Inflammation and Bone Density in Older Adults: What’s The Relationship?
Zoledronate Effective in Fracture Protection for Women with Osteopenia




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.