A systematic review published in World Journal of Gastroenterology observed a possible increased prevalence of osteoporosis in patients with Crohn’s disease compared with patients with ulcerative colitis or both conditions.
Researchers conducted a systematic review of population-based studies to assess the prevalence and development of osteoporosis and low bone mineral density (BMD) and its risk factors in patients with inflammatory bowel disease (IBD). Researchers assessed Embase and PubMed, as well as abstracts from 2014 to 2018 presented at the United European Gastroenterology Week, European Crohn’s and Colitis Organisation Congress, and Digestive Disease Week. Eligible studies investigated either the prevalence of osteoporosis or osteopenia and/or risk factors for osteoporosis or low BMD in patients with IBD. Studies on children under aged younger than 18 years were excluded.
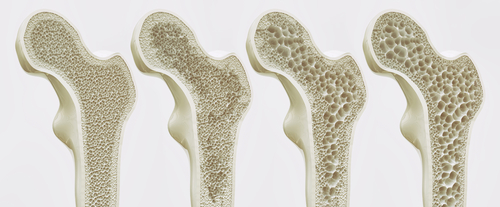
A total of 12 studies were included in the analysis, comprising 3,661 patients with IBD and 12,789 healthy controls. Prevalence of osteoporosis varied between 4% to 9% in studies that included patients with both Crohn’s disease and ulcerative colitis, between 2% to 9% in studies that included patients with ulcerative colitis only, and between 7% to 15% in studies that included patients with Crohn’s disease only. Among healthy controls, prevalence of osteoporosis was 3% and 10% in two studies.
A diagnosis of Crohn’s disease, lower body mass index (BMI), and lower body weight were risk factors associated with osteoporosis or low BMD. Patients with Crohn’s disease had an increased risk for osteoporosis or low BMD over time, while patients with ulcerative colitis did not. Increased age was associated with decreased BMD, and there was a positive association between weight and BMI and BMD over time. Outcomes related to patient sex were inconclusive.
Great heterogeneity was found in the included studies in terms of study methodologies, definitions, and the assessment of osteoporosis, and only a small number of population-based studies was available, the authors noted.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.