Among patients with coronavirus disease 2019 (COVID-19), those who are older and those with medical comorbidities or compromised immune systems are at increased risk for adverse outcomes. COVID-19 is caused by the novel acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Bassam G. Abu Jawdeh, MD, FASN, FAST, provided a review of outcomes of COVID-19 in kidney transplant recipients. The review, published in Advances in Chronic Kidney Disease [2020;27(5):383-389], focused on clinical characteristics and outcomes, immunosuppression management, and operational challenges facing transplant programs during the pandemic. To date, six retrospective studies from New York and Europe have reported on COVID-19 in kidney transplant recipients.
In one study of 36 patients, median age was 60 years, 72% were male, 39% were Black, and 75% received a deceased-donor transplant. The most common comorbidities were hypertension (94%), diabetes (69%), smoking (36%), and cardiovascular disease (17%). More than 85% were on mycophenolate/tacrolimus/prednisone maintenance immunosuppression and 42% received lymphocyte depleting induction. Twenty-eight patients were hospitalized; of those, all but one had radiologic evidence of a viral pneumonia. Of the patients with pneumonia, 11 required mechanical ventilation and six developed AKI that required renal replacement therapy. Of the 10 patients who died (median, 21 days), two were being monitored at home. Both were recent transplant recipients who received antithymocyte globulin within 5 weeks of presentation.
In a study at Columbia University of 15 kidney transplant recipients hospitalized with COVID-19, median age was 51 years, 65% were male, and 80% received a deceased-donor kidney transplant. Maintenance immunosuppression was primarily a regimen of an antimetabolite/tacrolimus/prednisone. The transplant program at Columbia adopts an early steroid-withdrawal strategy; however, the sample was enriched with patients on prednisone maintenance (67%), confirming the possible role of enhanced immunosuppression as a susceptibility factor.
Results of the early studies suggest that COVID-19 may present in an atypical manner in kidney transplant patients, with no fever, respiratory symptoms, or radiologic findings of pneumonia.
The optimal strategy for management of immunosuppression in transplant recipients with COVID-19 is unclear. Results of a study in cancer patients found that cancer patients with neutropenia have adverse outcomes, underscoring the role of the immune system in fighting the virus that causes COVID-19. Those results suggest the possibility of immunosuppression reduction to help alleviate the progression of SARS-CoV-2. However, that strategy may result in loss of the potential beneficial effect of immunosuppressive drugs in mitigating the systemic inflammatory response mediated by cytokine storm. In addition to antivirals, other strategies being investigated for the treatment of COVID-19 are adjunctive medications that target the inflammatory response, including glucocorticoids, interleukin-6 (IL-6) receptor antagonists, anticomplement-5 inhibitors, intravenous immunoglobulins, and mammalian target of rapamycin inhibitors that have been used for primary prevention and treatment of allograft rejection.
The role of diminished T-cell and B-cell immunity as a predisposing factor for severe infection is highlighted in the increased mortality among transplant recipients with COVID-19. However, to date, there is no level 1 evidence-based strategy to inform management of immunosuppression in that patient population. In patients with moderate disease, it may be reasonable to hold the antimetabolite and continue low-dose calcineurin inhibitor with or without glucocorticoids. In patients with severe disease and those who are critically ill, it may be justifiable to hold all maintenance immunosuppression and initiate remdesivir in addition to steroids.
Inflammatory biomarkers such as C-reactive protein, IL-6 levels, and ferritin have been shown to correlate with disease severity; albeit with substantial overlap and variability among patients. However, trending biomarkers in individual patients may play a role in guiding an immunosuppression reduction plan in those patients.
Challenges for Transplant Programs
Many kidney transplant programs suspended or limited operations during the COVID-19 pandemic. Concerns and challenges facing kidney transplant programs and practices are multifaceted.
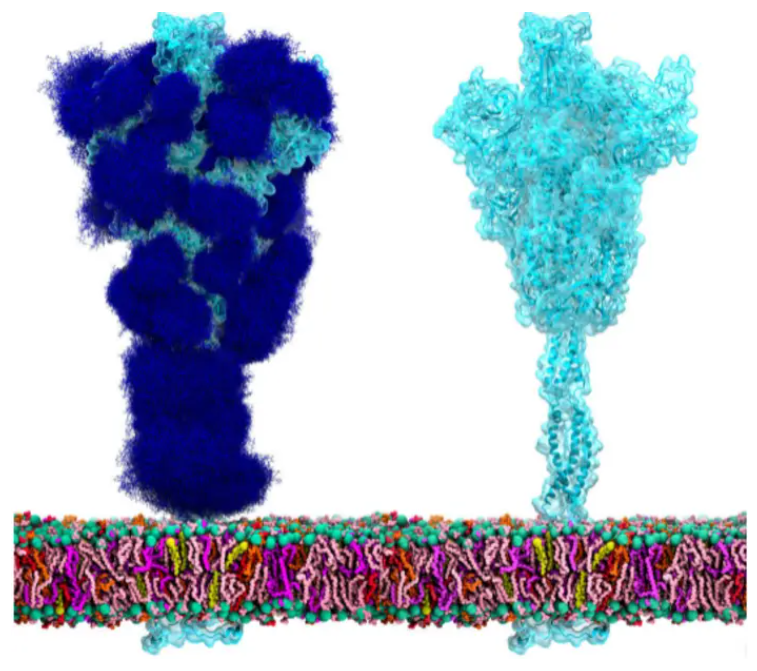
There is consensus that kidneys from deceased or living donors with confirmed infection of high risk of exposure to COVID-19 should not be used. While there are no data confirming donor to recipient viral transmission, the premise is plausible. There are three areas of concern: (1) the receptor that binds the spike protein of SARS-CoV-2 and facilitates its entry into targeted cells is angiotensin-converting enzyme 2; kidneys show the highest level of expression of the enzyme; (2) kidneys can be directly infected by SARS-CoV-2; and (3) SARS-CoV-2 viremia and viruria have been reported in 15% and 7% of COVID-19 patients, respectively.
Concerns are also related to the possibility of transplant team members as vectors of the virus. To date, 16% of all COVID-19 patients are healthcare workers; 29% of those had hospital-acquired infections. The possibility extends to organ procurement teams as well as transplant physicians and stresses the importance for appropriate physical distancing, hygiene, handwashing, and personal protective equipment for all team members.
In a survey of kidney transplant centers in the United States, 72% reported complete suspension of living donor transplant programs and 24% reported partial suspension of activities. Among deceased-donor programs, only 20% continued with no restrictions.
Most programs have adopted universal donor and recipient screening by nasopharyngeal nucleic acid testing (NAT) prior to transplantation. Only 17% of programs had blood NAT available to rule out viremia. For post-transplant care, 98% of centers limited in-person clinic visits and 97% reported adding telemedicine options.
In summary, the author said, “The COVID-19 pandemic has impacted transplantation and is associated with increased mortality among infected kidney transplant recipients. Without the availability of high-level evidence, most programs developed internal protocols to deal with new transplants and manage immunosuppression. Until effective therapies and a vaccine become available, we have to deal with this ‘new normal’ while taking care of our susceptible patient population. It is imperative for transplant providers to have a low threshold for suspecting SARS-CoV-2 infection and promptly initiate appropriate evaluation and immunosuppression reduction.”
Takeaway Points
- Coronavirus disease 2019 (COVID-19) is associated with adverse outcomes in kidney transplant recipients and has placed significant burden on kidney transplantation programs.
- Bassam G. Abu Jawdeh, MD, presented a review of COVID-19 and its impact in this patient population as well as challenges facing transplantation programs.
- Transplant providers should have a low threshold for suspected COVID-19 infections and steps in place for appropriate evaluation and reduction in immunosuppression in infected kidney transplant recipients.





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.