
Internal limiting membrane (ILM) peeling was discussed during several AAO 2019 presentations.
The first was a scientific poster that analyzed the use of the Preceyes Surgical Robotic System versus manual ILM peeling via the EYESi (VRmagic) surgical simulator. For the comparison, 23 vitreoretinal surgeons performed a manual procedure followed by a robotic one. Prior to the robotic procedure, all surgeons received a 15-minute introduction, including time to practice instrument movements. An odometer was used to measure intraocular instrument movement. ILM peeling took an average of five minutes using the manual approach versus nine minutes with the robot (paired t test, P=0.002). Intraocular instrument movement using the robot was about half of that of the manual approach. There were 32 macular retinal hemorrhages in the robot group compared to 53 in the manual group (Mann-Whitney U test, P=0.035). The use of the robot eliminated retinal injuries.
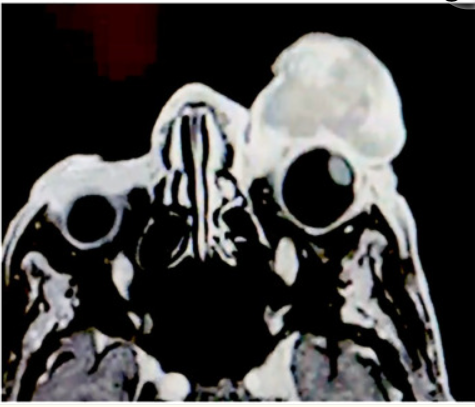
The second was also a scientific poster in which presenters discussed the anatomical and functional outcomes of ILM peeling with pas plana vitrectomy (PPV) to treat pediatric patients with rhegmatogenous retinal detachment (RRD). This was a retrospective interventional case series involving RRD patients aged ≤ 18 years who underwent combined lensectomy and PPV with extended ILM peeling. Among the 34 eyes included in the study, RRD etiology was primarily traumatic (32.4%) and equally myopic and developmental anomaly (26.5% each). Most patients (88.2%) had proliferative vitreoretinopathy grade C or worse. ILM peeling went to the equator. Patients were followed for a mean 18 months. At final follow-up, 38.2% of patients achieved final corrected distance visual acuity better than 20/200. Initial retinal reattachment was 55.9%; final anatomical success was achieved in most cases (88.2%).
Finally, a scientific poster detailed ILM peeling outcomes associated with different areas in idiopathic macular hole (IMH) surgery. This randomized clinical trial included 121 eyes that underwent vitrectomy. ILM was randomized to be peeled with two disc diameters (2 DD) or four disc diameters (4 DD). The primary outcome was 12-month closure rate; the secondary outcome was closure rate after stratification by macular hole closure index (MHCI). At 12-month follow-up, 82.5% of 2 DD eyes (n = 52/63) and 91.4% of 4 DD eyes (n = 53/58) achieved closure—a difference of –8.8%, which the researchers said did not signify inferiority of the 2 DD group compared to the 4 DD group (P=0.15). In an analysis of patients with MHCI ≤ 0.5, the 2 DD group had a significantly lower closure rate (18.2%) than the 4 DD group (75.9%; P=0.012); closure rates were similar among patients with MHCI > 0.5 (96.2% vs. 95.6%, respectively; P=0.185).






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.