
A study published in the Journal of Gastroenterology and Hepatology found that
Helicobacter pylori (H. pylori) infection was associated with an approximately 25% increased risk of osteoporosis, regardless of risk factors and confounding factors.
The longitudinal, retrospective cohort study included 10,482 women (mean age, 50.2 years) without osteoporosis at baseline. South Korean participants underwent a repeated health‐screening examination, including an H. pylori‐specific immunoglobulin G antibody test and dual-energy X-ray absorptiometry (DXA; to diagnose osteoporosis), from January 2000 to December 2019.
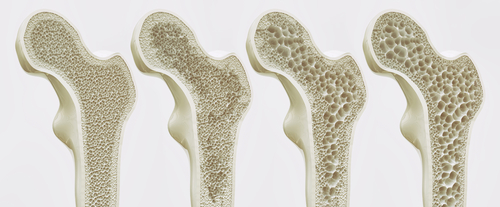
The baseline prevalence of H. pylori infection was 57.3% (n=6,009). During 77,515.3 person‐years of follow‐up, women with H. pylori infection had a higher rate of incident osteoporosis than those without H. pylori. Per multivariable assessment that adjusted for age, body mass index (BMI), menopausal status, smoking status, regular exercise, comorbidities (including hypertension, diabetes, dyslipidemia, stroke, or ischemic heart disease), and concomitant medications, the hazard ratio (HR) for incident osteoporosis in women with H. pylori infection was 1.23 compared with women without infection (95% confidence interval [CI], 1.03-1.45).
There was also an observed association between H. pylori and development of osteopenia. Significant risk factors for osteoporosis included menopause (HR, 1.68; 95% CI, 1.31-2.16) and increasing age (HR, 1.07; 95% CI, 1.06-1.08). However, higher BMI (HR, 0.84; 95% CI, 0.81-0.87) was a protective factor for the risk of osteoporosis.
“Physicians should pay more attention to women with H. pylori infection by using DXA scan, especially in postmenopausal women or women with lower BMIs,” the authors concluded.




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.