In a single-arm phase I/II study, infusion with CT103A, a novel fully human B-cell maturation antigen (BCMA)-targeted chimeric antigen receptor (CAR) T-cell therapy, led to rapid and durable responses in patients with heavily pretreated relapsed/refractory multiple myeloma. These outcomes were seen even among patients with prior anti-BCMA CAR T-cell exposure, the authors reported in their presentation at the 63rd American Society of Hematology Annual Meeting and Exhibition.
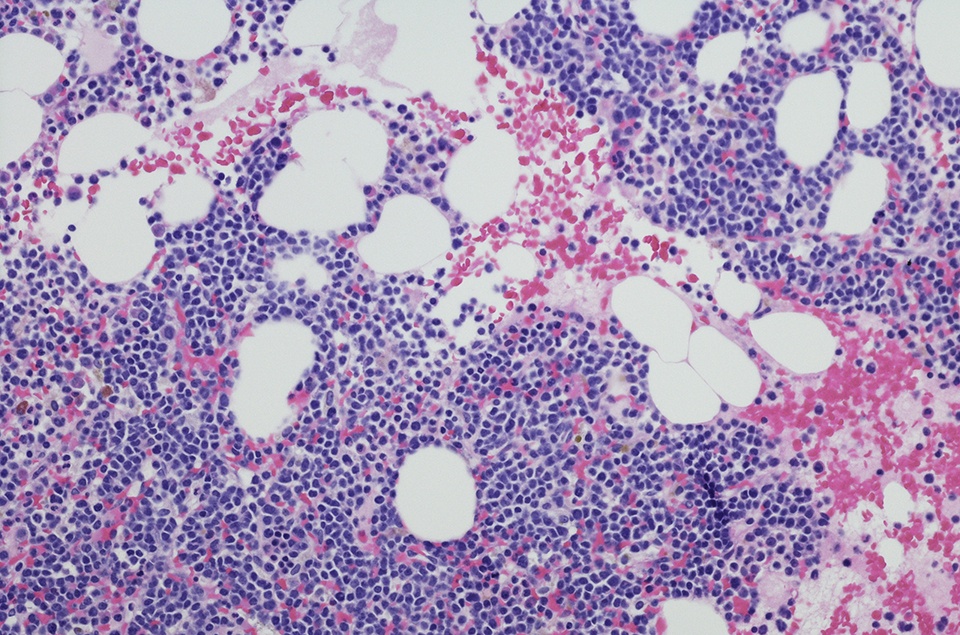
A total of 71 patients had received CT103A infusion: nine in phase Ia, 17 in phase Ib, and 45 in phase II. The median age was 58.0 years (range = 41-71) and 59.2% of patients were male. Eligible patients received at least three previous lines of therapy, including a proteasome inhibitor and an immunomodulator, and were refractory to their last treatment. Patients received a median of four (range = 3-13) prior lines of therapy, including previous autologous stem cell transplantation (28.2%), anti-CD38 antibodies (18.3%), and notably, CAR T-cell therapy (18.3%). Seven percent of patients had extramedullary disease at baseline and 76.1% had high-risk cytogenetics.
Median follow-up was 147 days (range = 31-1,029). The recommended phase II dose was 1.0×106 CAR T cells/kg. Patients underwent lymphodepletion with fludarabine and cyclophosphamide prior to infusion. Hematologic toxicities were the most common grade ≥3 treatment-related adverse events (AEs). Most patients (93%) experienced cytokine release syndrome (2.8% grade ≥3) after a median of six days, although all cases were relieved after conventional intervention. One patient experienced immune effector cell-associated neurotoxicity syndrome and recovered without intervention.
All patients were evaluable for at least one month of follow-up. The median time to treatment response was 15 days, with a 94.4% overall response rate (ORR). Half of patients (50.7%) achieved at complete response (CR) or better. Twenty-seven percent of patients achieved a very good partial response (VGPR) and 16.9% had a partial response (PR).
In a subgroup of 50 patients with at least three months of follow-up, the ORR was 96.0%, with 54.0% ≥CRs, 28% VGPRs, and 14% PRs. Among the patients with previous CAR T-cell exposure, the ORR was 76.9%, with 38.5% ≥CRs, 15.4% VGPRs, and 23.1% PRs.
Measurable residual disease (MRD) status was assessed in 69 patients, and 92.8% achieved MRD-negativity within a median of 17 days (range = 13-180). Three-quarters of MRD-negative patients sustained negativity status over six months.
CT103A expansion peaked at a median of 12 days (range = 5-29) and was still detectable in 23 of 26 (88.5%) patients with six-month follow-up and 14 of 16 patients (87.5%) with one year follow-up. The researchers also noted that the first enrolled patient “remains in [sustained complete remission] for 34 months with significant persistence of CT103A transgene.”
“The impressive efficacy of CT103A, including time to response, overall response rate, and durability, was corroborated by robust expansion and prolonged persistence of CT103A,” the authors concluded. “The expansion and clinical benefits of CT103A did not seem to be influenced by prior murine BCMA CAR T cells.”




 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.