Hemodynamic Evaluation of Cardiogenic Shock With Dr. Nosheen Reza
By CardioNerds - Last Updated: August 1, 2023The hemodynamic evaluation of cardiogenic shock obtained via a Swan-Ganz catheter plays an essential role in the characterization of cardiogenic shock patients.
Join Dr. Nosheen Reza, Assistant Professor of Medicine and Advanced Heart Failure and Transplant cardiologist at the Hospital of the University of Pennsylvania, Dr. Brian McCauley, Interventional and Critical Care Fellow at the Hospital of the University of Pennsylvania, Dr. Mark Belkin, Cardiac Critical Care Series Co-Chair and AHFT fellow at University of Chicago, and CardioNerds Co-Founders, Drs. Amit Goyal and Daniel Ambinder, for this tour through the heart aboard the Swan-Ganz catheter.
In this episode, we evaluate three separate admissions for a single patient to highlight pearls regarding waveform assessment, evaluating cardiac output, phenotyping hemodynamic profiles, targeted therapies based on hemodynamics, and more.
Episode introduction and audio editing by Dr. Gurleen Kaur, Director of the CardioNerds Internship.
Pearls and Quotes
1. Swan-Ganz catheters are not dead #ReviveTheSwan! They remain a useful tool to characterize cardiac patients & to help direct therapy, especially in Cardiogenic Shock.
2. When looking at Swan-Ganz catheter data, it is important to always interpret your own tracings, to know what values are acquired directly, and which values are derived.
3. It is important to understand the strengths and weakness of hemodynamic characterization by Swan-Ganz catheters.
4. Advanced metrics such as cardiac power output, pulmonary artery pulsatility index, and aortic pulsatility index are extremely useful in further phenotyping patients as well as guiding mechanical support platforms.
5. “The data will be wrong if the preparation is not right.”
Show Notes
1. Swan-Ganz catheters are a useful tool to characterize cardiac patients and to direct therapy.
• With the ESCAPE trial in 2004, Swan-Ganz catheter utilization dropped drastically outside transplant centers across the United States (2).
• While the ESCAPE trial did demonstrate the possibility of harm when using a Swan-Ganz catheter, many of the truly ill cardiac patients we care for would have been excluded from the trial. For instance, patients on dobutamine at doses above 3 µg/kg/min or any dose of milrinone during the hospitalization were excluded from the trial.
• This is a classic example of “throwing the baby out with the bath water.”
• In a recent large, multicenter cardiogenic shock registry, complete hemodynamic assessment using pulmonary artery catheters prior to MCS is associated with lower in-hospital mortality compared with incomplete or no assessment (3).
2. When looking at Swan-Ganz catheter data, it is important to always interpret your own tracings, to know what values are acquired directly, and which values are derived.
• Incomplete or incorrect data can lead to mischaracterization of our patients.
• Therefore, it is essential to review all of the tracings, calculations, and data acquired for each individual patient before any clinical adjustments are made (1).
• An incomplete pulmonary capillary wedge tracing is an example from clinical practice (causing the PCWP, and therefore the left-sided filling pressures to be overestimated). It is equally important to know the limitations of cardiac output equations, and that no one measurement is perfect.
• Foibles of the Fick equation include assumed rather than measured oxygen consumption and variations in hemoglobin concentration.
• Traditionally, thermodilution has been thought to be likely less accurate in presence of tricuspid regurgitation, which could lead to blending of the cold dilutant, but recent data suggests even in these circumstances it remains the preferred method for estimating cardiac output over indirect Fick.
3. What are some tips of measuring a PCWP correctly?
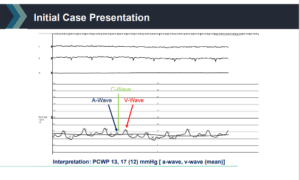
• To ensure that we get the wedge pressure correctly, we must first make sure we understand the wedge pressure in relation to the respiratory cycle. For the majority of patients, the end expiratory intrathoracic pressure will be close to 0, and it will have the least influence on our readings. Thus, for most patients, that is why we measure the wedge pressure at end expiration.
• However, in patients with severe lung disease or significant obesity, the intrathoracic pressure may not be close to 0 at end expiration or there may be wide swings in intrathoracic pressure. For these patients, it is a reminder to look at the tracings yourself, and we may need to average the PCWP over the respiratory cycle.
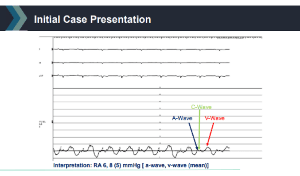
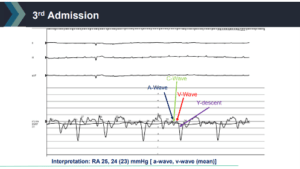
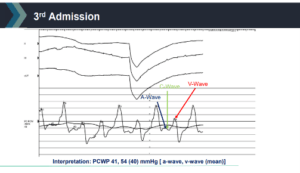
• When we are measuring the PCWP, we have to remember that we are using it as a surrogate of the LV end-diastolic pressure. The point of the cardiac cycle when the pressure in the pulmonary veins, left atrium and LV are closest to equal is end-diastole. Thus, we typically want to measure the PCWP in end-diastole, which would specifically be measuring the mean of the A-wave.
• Now, for patients with severe mitral regurgitation and/or significant atrial myopathy leading to large V-waves, the wedge pressure estimated at end-diastole will not necessarily reflect the mean wedge (averaged throughout the cardiac cycle) that the pulmonary circulation “sees” throughout the cardiac cycle. As has been a theme in this episode, we have to make sure our inputs are accurate to appropriately help our patients. In this circumstance of large V-waves, if we were calculating the pulmonary vascular resistance (Mean PA Pressure – PCWP / CO) but used the end-diastolic PCWP instead of the PCWP averaged through the cardiac cycle we may end up with an inaccurate estimation of PVR.
4. Advanced metrics such as cardiac power output, pulmonary artery pulsatility index, and aortic pulsatility index are extremely useful in further characterizing hemodynamics.
• Over the past several years individual indices of ventricular performance have been developed and studied, these include CPO, PAPi, API, and LVSWI (4,5,10-12). These values can further flesh out our hemodynamic profiles and help guide decision-making for choosing the proper mechanical circulatory support platform (7,8,9).
• See the infographic developed by CardioNerds Academy Fellow Ahmed Ghoneem for more information on different thresholds for these parameters.
• The API is a novel hemodynamic parameter that was recently applied to ESCAPE trial patients by series Co-Chair, Mark Belkin.
5. “The data will be wrong if the preparation is not right.”
• Dr. Reza’s point on the episode is apt and high-yield.
• Incorrect data acquisition and/or interpretation will not benefit our patients. We need to know what values are measured directly (chamber pressures, SvO2) and which are derived (cardiac output/index, SVR/PVR, CPO/PAPi/API, and so forth).
• As cardiologists and intensivists, we need to be critical of the tracings themselves, avoid anchoring to a single value, and be observant of the overall hemodynamic trajectory our patient is taking.
• Only through thoughtful intervention in coordination with careful and consistent monitoring will we bring to bear the benefits bestowed by Swan-Ganz catheter supplemented-care (1).
Schematics and Graphics
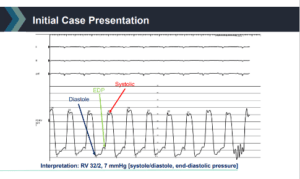
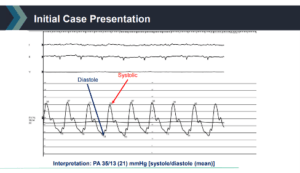
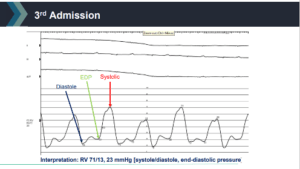
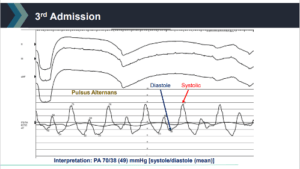
RHC Tracings Discussed in the Episode
References
1. Ragosta M. Textbook of Clinical Hemodynamics. Elsevier; 2017.
2. Binanay C, Califf RM, Hasselblad V, et al. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005;294(13):1625-33. https://jamanetwork.com/journals/jama/fullarticle/201634
3. Garan AR, Kanwar M, Thayer KL, et al. Complete hemodynamic profiling with pulmonary artery catheters in cardiogenic shock is associated with lower in-hospital mortality. JACC Heart Fail. 2020;8(11):903-913. https://pubmed.ncbi.nlm.nih.gov/33121702/
4. Korabathina R., Heffernan K.S., Paruchuri V., Patel A.R., Mudd J.O., Prutkin J.M., et al: The pulmonary artery pulsatility index identifies severe right ventricular dysfunction in acute inferior myocardial infarction. Catheter Cardiovasc Interv 2012; 80: pp. 593-600. https://pubmed.ncbi.nlm.nih.gov/21954053/
5. Fincke R, Hochman JS, Lowe AM, et al. Cardiac power is the strongest hemodynamic correlate of mortality in cardiogenic shock: a report from the SHOCK trial registry. J Am Coll Cardiol. 2004;44(2):340-8. https://pubmed.ncbi.nlm.nih.gov/15261929/
6. Kochav SM, Flores RJ, Truby LK, Topkara VK. Prognostic impact of pulmonary artery pulsatility index (Papi) in patients with advanced heart failure: insights from the escape trial. J Card Fail. 2018;24(7):453-459. https://pubmed.ncbi.nlm.nih.gov/29597051/
7. Feldman D, Naidu SS. Percutaneous Mechanical Circulatory Support Devices. Cardiac Interventions Today. 2016; 10 (1): 26-33. https://citoday.com/articles/2016-jan-feb/cover-stories
8. Briceno N, Kapur NK, Perera D. Percutaneous mechanical circulatory support: current concepts and future directions. Heart. 2016;102(18):1494-507. https://pubmed.ncbi.nlm.nih.gov/27503999/
9. Baran DA, Grines CL, Bailey S, et al. Scai clinical expert consensus statement on the classification of cardiogenic shock: this document was endorsed by the american college of cardiology (Acc), the american heart association (Aha), the society of critical care medicine (Sccm), and the society of thoracic surgeons (Sts) in April 2019. Catheter Cardiovasc Interv. Published online May 19, 2019:ccd.28329. https://pubmed.ncbi.nlm.nih.gov/31104355/
10. Drazner MH, Velez-Martinez M, Ayers CR, et al. Relationship of right- to left-sided ventricular filling pressures in advanced heart failure: insights from the ESCAPE trial. Circ Heart Fail. 2013;6(2):264-270. https://pubmed.ncbi.nlm.nih.gov/23392790/
11. Belkin MN, Alenghat FJ, Besser SA, et al. Aortic pulsatility index predicts clinical outcomes in heart failure: a sub-analysis of the ESCAPE trial. ESC Heart Fail. 2021;8(2):1522-1530. https://pubmed.ncbi.nlm.nih.gov/33595923/
12. Belkin MN, Kalantari SA, Kanelidis AJ, et al. Aortic Pulsatility Index: A Novel Hemodynamic Variable for Evaluation of Decompensated Heart Failure. J Card Fail. 2021;27(10):1045-1052. https://pubmed.ncbi.nlm.nih.gov/34048919/



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.