An article in Thoracic Cancer reported that dual high expression of T cell immunoreceptor with immunoglobulin and ITIM domains (TIGIT) and cluster of differentiation 47 (CD47) was associated with a poor prognosis in patients with lung squamous cell carcinoma (LUSC). The study was performed by investigators, led by Yue Peng, from the National Clinical Research Center for Cancer at the Chinese Academy of Medical Sciences & Peking Union Medical College in Beijing, China.
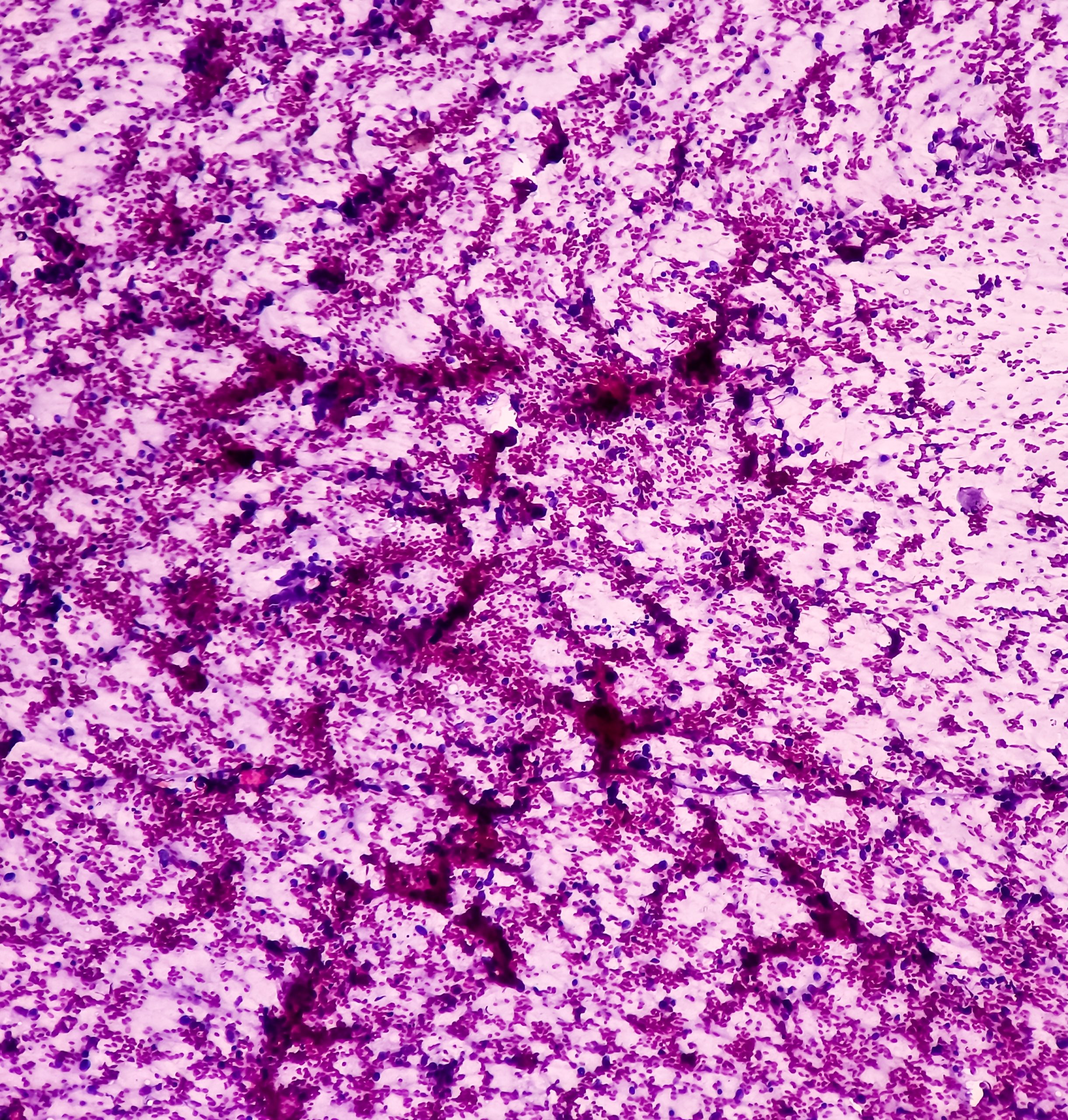
The trial included clinical information from a total of 190 retrospective patients with LUSC who underwent surgical treatment at the authors’ center. Immunohistochemical staining was used to assess TIGIT and CD47. The authors also obtained transcriptional and clinical data of 479 LUSC samples from The Cancer Genome Atlas (TCGA) as a secondary cohort.
LUSC TIGIT and CD47 Expression Profile Results
In the TCGA cohort, the authors observed dual high expression of TIGIT and CD47 at the RNA level in 142 (29.6%) cases, and further noted that the expressions were significantly correlated with each other (p <0.001). Greater proportions of female cases exhibited high TIGIT (p = 0.001) and high TIGIT/CD47 (p = 0.049) dual expression, according to the report. Advanced TNM stage (p = 0.006) and high TIGIT/CD47 (p = 0.047) dual expression were both predictive markers for LUSC.
In the 190 cases from the authors’ center, 75 (39.5%) had dual high expression of TIGIT/CD47. The correlation between the two genes was observed in this cohort as well. Other independent prognostic factors identified in this cohort included older age (p = 0.001), advanced TNM stage (p <0.001), and TIGIT/CD47 dual high expression (p = 0.046).
Authors noted that, while they presented TIGIT and CD47 as potential predictors of treatment response, their analysis did not included treated patients. As such, they could not make any inferences about the prediction of efficacy.
Overall, Peng and colleagues proposed that “patients with dual high expression of CD47/TIGIT might be suitable for new target immunotherapy in the future.”
Visit the Lung Cancer Resource Center for more recent research.






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.