Patients with atherosclerotic peripheral arterial disease (PAD) have marked increases in coagulability, defined as coagulation factor activity and hemostatic markers of endothelial dysfunction, according to a new study published in Vascular Specialists International. Hypercoagulability was made worse by performance of invasive procedures, and the increased activity of coagulation factors and hemostatic markers was associated with PAD complications.
“Assessment of the pathogenesis of thrombotic complications in patients with PAD may provide insight into the future possible application of alternative antithrombotic therapies,” wrote the study authors.
Relationship Between Coagulability and PAD
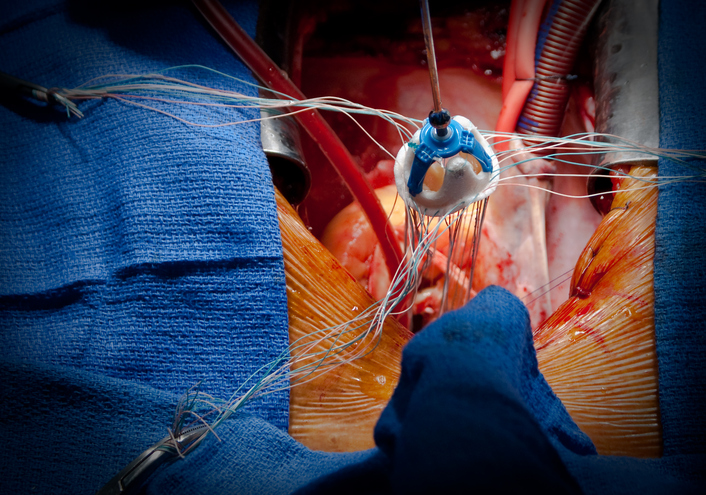
The investigators prospectively enrolled 120 patients aged ≥40 years with Fontaine stages 2b to 3 PAD. Patients underwent either open surgical (n = 40), endovascular (n = 40), or conservative (n = 40) treatment for PAD. The surgical treatment group underwent a bypass procedure with synthetic grafts of polytetrafluoroethylene or polyester. Endovascular treatment consisted of angioplasty or bare metal nitinol stenting. Conservatively treated patients received antiplatelet drugs and statins. All patients received dual antiplatelet treatment (aspirin and clopidogrel) for 12 months. Patients requiring anticoagulant therapy were excluded.
The investigators evaluated coagulation factors (FVIII, FIX, and FXI) and endothelial markers, including:
- von Willebrand factor (vWF) activity
- soluble endothelial protein C receptor (sEPCR)
- plasminogen activator inhibitor-1 (PAI-1) levels
Increased Activity After Three Months
At baseline, patients who were treated for their PAD with open surgery had higher activity of vWF, FVIII, FIX, and FXI, and higher levels of PAI-1 and sEPCR. This trend was consistent at three months. In addition, at three months patients in the open surgery group had a significant increase in FVIII activity from baseline (175% to 233%; P < 0.001).
Five patients who underwent bypass had disease progression at 12 months; these patients also had statistically significant increases in vWF activity (P = 0.027) and nitric oxide (NO) metabolites (P = 0.014) at three months compared to baseline. Six bypass patients with increased FVIII activity developed graft thrombosis in the early postoperative period, leading to amputation. The authors note, however, “we cannot completely rule out the possibility of technical failure due to overestimation of distal runoff and technical difficulties while performing distal anastomosis.”
Similarly to the open surgery group, the endovascular treatment group had increased activity of vWF, FVIII, FIX, and FXI and higher levels of PAI-1 and sEPCR compared to normal values. After three months, increases were seen for activity in FVIII (157% to 184%), FIX (180% to 218%), and FXI (156% to 181%; all P<0.05). One patient in this group, who had increased activity of both coagulation factors and hemostatic markers, developed thrombosis. Four patients (10%) with baseline increased vWF activity developed myocardial infarction and received percutaneous coronary interventions. Six patients with restenosis had baseline increased vWF and decreased NO levels that continued after three months.
In the conservative treatment group, three patients with increased activity of vWF later developed myocardial infarction (P = 0.049), and three patients with increased PAI-1 activity developed PAD progression after treatment (P = 0.028).
A multiple logistic regression analysis found that elevated FVIII activity (P = 0.005) and sEPCR levels (P = 0.027) were associated with higher risk of peripheral arterial thrombosis. The investigators also found an association between decreased sEPCR and NO levels and increased risk of stenosis in one year for patients who received endovascular treatment (all P < 0.05).
“The activities of intrinsic coagulation factors and hemostatic markers of endothelial dysfunction were increased in patients with advanced atherosclerotic PAD. Invasive treatment, including open or endovascular procedures, promotes further hypercoagulability,” wrote the authors in summary. “Increased activity of coagulation factors and altered levels of hemostatic markers of endothelial dysfunction were associated with PAD complications such as graft thrombosis, myocardial infarction, disease progression, and restenosis.”






 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.