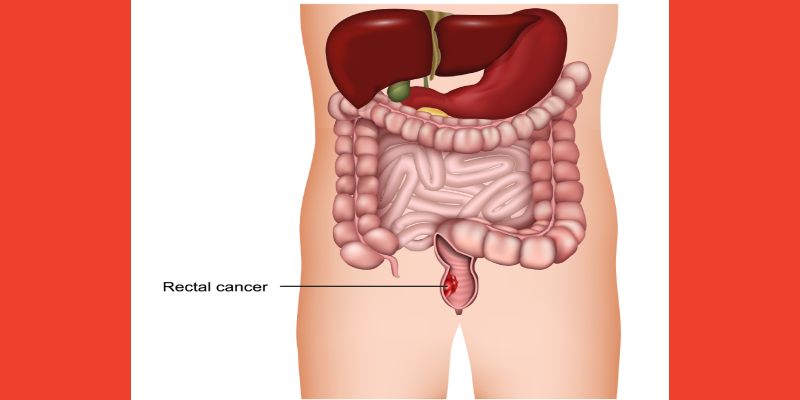
Total neoadjuvant therapy (TNT) with induction chemoimmunotherapy followed by long-course chemoradiation may lead to high complete response (CR) and organ preservation rates in patients with high-risk rectal cancer and proficient mismatch repair (pMMR) status, according to new research published in JAMA Surgery.
TNT is considered standard of care for locally advanced rectal cancer, especially for patients with high-risk factors. The effectiveness of TNT combined with immunotherapy for patients with pMMR rectal cancer is yet to be fully understood.
Yingjie Li, MD, of Peking University Cancer Hospital and Institute, and colleagues designed a cohort study to evaluate the safety and efficacy of TNT with induction chemoimmunotherapy followed by long-course chemoradiation in patients with high-risk, pMMR rectal cancer. They also sought to identify potential molecular biomarkers associated with treatment efficacy.
The single-arm, phase 2 study enrolled 25 patients at the Gastrointestinal Cancer Center at Peking University Cancer Hospital and Institute from June 2020 to October 2021. Patients received 3 cycles of induction oxaliplatin and capecitabine combined with camrelizumab and radiotherapy (50.6 Gy in 22 fractions) with concurrent capecitabine. Those patients without disease progression received 2 cycles of consolidation oxaliplatin and capecitabine.
Researchers collected biopsies and plasma before treatment for whole-exome sequencing and cell-free DNA sequencing, respectively.
Twenty-two of the patients enrolled completed the TNT schedule, among whom the pathologic CR was 33.3%. Twelve (48%) patients achieved clinical CR and 4 (16%) chose to watch and wait.
Dr. Li and colleagues noted that R0 resection was achieved in 21 of 21 eligible patients, and the major pathologic response rate was 38%.
The most common adverse event (AE) in this patient sample was nausea (80%), and 36% of patients experienced grade 3 AEs.
Notably, patients with tumor shrinkage of at least 50% after induction with oxaliplatin and capecitabine combined with camrelizumab, or those who experienced clinical CR, were more likely to have LRP1B mutation. Researchers reported that LRP1B mutation was associated with high tumor mutation burden as well as tumor neoantigen burden, and those patients with high tumor mutation burden benefited from therapy.
“This study found that TNT with induction chemoimmunotherapy followed by long-course chemoradiation was safe and effective for patients with high-risk rectal cancer with pMMR status,” study authors concluded, adding that longer follow-up and larger clinical studies are needed to validate this finding. “There is also an urgent need to further validate the predictive value of LRP1B and discover other novel biomarkers with potential predictive value for rectal cancer.”



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.