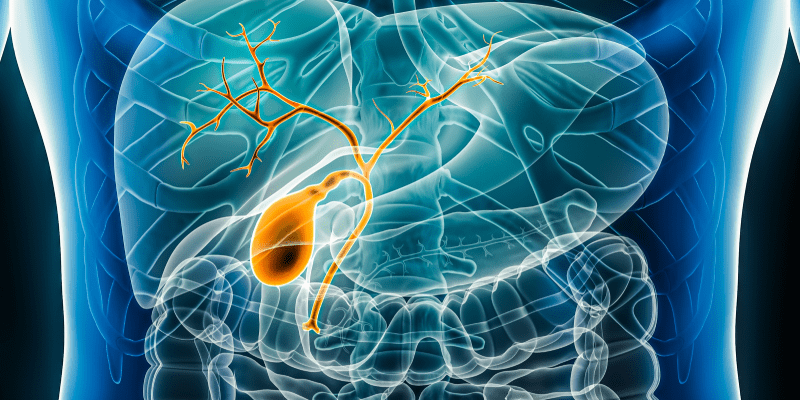
Tumor budding (TB) is a prognostic factor that is often indicative of an aggressive tumor. In several different types of cancer including intrahepatic cholangiocarcinoma (iCCA), it is linked to poor survival outcomes.
Tumor histomorphological features are often altered after patients undergo neoadjuvant chemotherapy (NAC), as treatment can cause shrinkage of tumor cells, collagenization, necrosis, and more. As a result, a recent study has sought to determine the prognostic significance of TB in patients with iCCA both before and after undergoing NAC according to the modified International Tumor Budding Consensus Conference (ITBCC) criteria.
The study enrolled patients with iCCA who had received treatment with NAC, and analyzed each patient’s biopsy and surgical resection samples. Out of 147 total patients included in the study, 95 cases of biopsy material were obtained prior to NAC, while 139 cases of post-NAC resection with viable tumor cells were examined for TB assessment.
The post-treatment analysis excluded 5 cases that showed complete tumor necrosis and 3 cases of resection that were not available; a total of 87 cases had paired pre- and post-NAC biopsy and resection specimens for TB assessment.
The median follow-up time was 29 months, during which 79 patients (53.7%) developed disease progression and 32 patients (21.8%) died. Biopsy specimens obtained before NAC showed that the TB-positive subgroup had a lower overall survival (OS) rate at univariate analysis (P=.010). In resection specimens taken after NAC, the TB-positive subgroup had reduced OS (P=.002) and recurrence-free survival (RFS) (P=.013) in univariate analysis.
When considering TNM stage, lymphovascular invasion, and perineural invasion, a TB-positive status post-NAC served as an independent prognostic factor for both OS and RFS (OS, HR, 3.005; 95% CI, 1.333–6.775, P=.008; RFS, HR, 1.748; 95% CI, 1.085–2.816, P=.022).
Tumor regression scores did not show significant association with TB grade (P=.395), and grade 3 scores did not show a significant association with either OS (P=.870) or RFS (P=.205) at univariate analysis, as well as on Kaplan–Meier curves for either OS (P=.382) or RFS (P=.052).
Overall, determining the presence of TB in patients with iCCA can provide additional context when considering NAC for patients, and can potentially be included in routine pathological reporting.



 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.