
New study results presented at the American Heart Association 2019 Scientific Sessions in Philadelphia suggest that an invasive interventional approach for treating stable ischemic heart disease yields no reduction in risk when compared to a less invasive approach.
“It is unknown whether a routine invasive approach of cardiac catheterization and revascularization offers incremental value over a conservative approach of optimal medical therapy (OMT), with catheterization reserved for failure of medical therapy in patients with stable ischemic heart disease (SIHD) and moderate or severe ischemia,” the authors explained in their rationale.
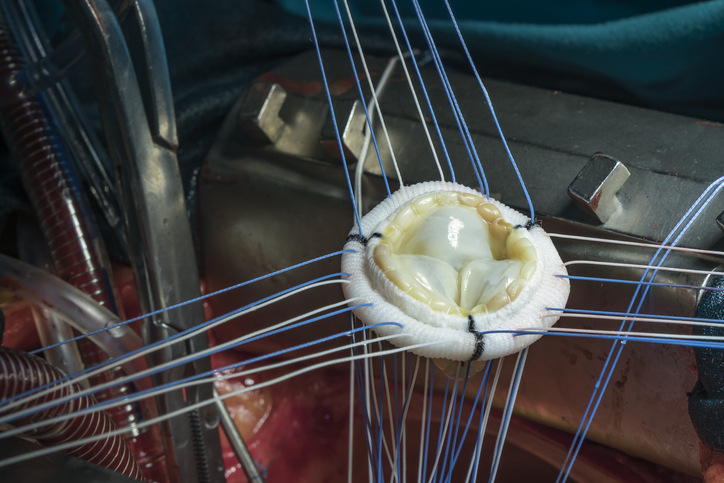
The International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA) study included patients with estimated glomerular filtration rate (eGFR) <30 mL/min, recent myocardial infarction (MI), left ventricular ejection fraction (LVEF) <35%, left main stenosis >50%, or unacceptable angina at baseline. Patients were randomized to receive either an invasive approach consisting of routine cardiac catheterization followed by revascularization with percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG; n=2,588), or a conservative approach in which patients underwent cardiac catheterization only if OMT failed (n=2,591). All patients received secondary prevention that included lifestyle and pharmacologic interventions as well. The primary study endpoint was a composite of cardiovascular (CV) death, myocardial infarction (MI), resuscitated cardiac arrest, or hospitalization for unstable angina or heart failure. Major secondary endpoints included CV death and MI.
According to the study results, there were no significant differences in the primary study outcome between the invasive and conservative groups (adjusted HR=0.93; 95% CI, 0.80 to 1.08; P=0.34) during study follow-up. There was also no difference between the groups for the secondary endpoints of CV death and MI (adjusted HR=0.90; 95% CI, 0.77 to 1.06; P=0.21). There was no net clinical benefit for the invasive approach vs. the conservative approach for CV death, MI, unstable angina, heart failure, resuscitated cardiac arrest, or stroke (adjusted HR=0.95; 95% CI, 0.82 to 1.10; P=0.50). When broken down by type of MI, there was a reduction in Type 4a or 5 MI with the invasive group (adjusted HR=2.98; 95% CI, 1.87 to 4.74; P<0.01), and a reduction in spontaneous type 1, 2, 4b or 4c MI (adjusted HR=0.67; 95% CI, 0.53 to 0.83; P<0.01).
“ISCHEMIA is the largest trial of an invasive vs. conservative strategy for patients with SIHD,” presenter Judith S. Hochman, MD, of the NYU School of Medicine, said in her presentation. “Overall, an initial invasive strategy as compared with an initial conservative strategy did not demonstrate a reduced risk over media 3.3 years for the primary endpoint (CV death, MI, hospitalization for unstable angina, heart failure, or major secondary endpoints of CV death or MI).”





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.