Highlights
- Researchers compared almost 8,000 patients from four studies for safety and efficacy of dual vs. triple therapy in AFib after PCI.
- Dual therapy consisted of a direct oral anticoagulant plus a P2Y12 inhibitor, and triple therapy included a vitamin K antagonist, aspirin, and a P2Y12 inhibitor.
- Dual therapy was more effective at reducing bleeding than triple therapy in these patients, but was inconclusive on other endpoints like all-cause mortality, stroke, and more.
A new meta-analysis suggests that dual antiplatelet therapy is more effective than triple antiplatelet therapy for reducing bleeding in patients with atrial fibrillation (AFib) after percutaneous coronary intervention (PCI).
The analysis, published in the Annals of Internal Medicine, looked at the safety and efficacy of dual therapy (direct oral anticoagulant plus a P2Y12 inhibitor) compared with triple therapy (a vitamin K antagonist plus aspirin plus a P2Y12 inhibitor) in a study cohort of patients with non-valvular AFib after PCI. They drew upon randomized controlled trials that compared effects of dual and triple therapy on endpoints like bleeding, mortality, and ischemic events in adults with AFib following PCI.
The study ended up including four trials (n=7,953). At one year media follow-up, the authors reported high-certainty evidence that dual therapy was associated with a reduction in risk for major bleeding compared with triple therapy (risk difference, −0.013; 95% CI, −0.025 to −0.002). For all-cause mortality (risk difference, 0.004; 95% CI, −0.010 to 0.017), cardiovascular mortality (risk difference, 0.001; 95% CI, −0.011 to 0.013), myocardial infarction (risk difference, 0.003; 95% CI, −0.010 to 0.017), stent thrombosis (risk difference, 0.003; 95% CI, −0.005 to 0.010), and stroke (risk difference, −0.003; 95% CI, −0.010 to 0.005), low-certainty evidence was inconclusive for dual vs. triple therapy. The researchers cited the heterogeneity of study designs, difference in dosages, and the different types of P2Y12 inhibitors as limitations in the study.
“In adults with AFib after PCI, dual therapy reduces risk for bleeding compared with triple therapy, whereas its effects on risks for death and ischemic end points are still unclear,” the analysis authors wrote in their conclusion.
In an accompanying editorial, the authors likened the choosing the right therapy track to an ancient story.
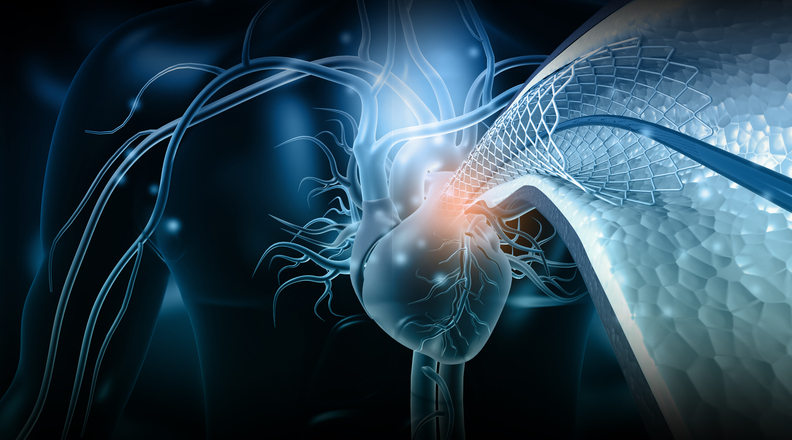
“In The Odyssey, Ulysses navigates between 2 hazards, a rock shoal commandeered by a 6-headed monster (Scylla) and a whirlpool known for gobbling up ships and claiming their crews (Charybdis),” they wrote. “The more he tries to avoid one hazard, the more vulnerable he becomes to the other. We face an analogous situation when caring for patients with atrial fibrillation (AF) after coronary stent placement who require anticoagulation to mitigate stroke risk and antiplatelet therapy to promote stent patency. We want to avoid bleeding events—which are increased with combination therapy—while also avoiding ischemic events, such as stent thrombosis, myocardial infarction, and ischemic stroke.”
Excellent paper in @AnnalsofIM regarding dual versus triple therapy for Afib after PCI led by @safinmc. Accompanying editorial discusses the difference between our and the recent @ESC_Journals @ehj_ed meta analysis. @ErinMichos @mmamas1973 https://t.co/kOsXevMZYX
— Shahzeb Khan (@ShahzebKhanMD) March 16, 2020
https://twitter.com/ErinMichos/status/1239694278915284992
Dual Versus Triple Therapy for #AFIB and #PCI – Review
Key Take-Home:
– only 4 trials met criteria
– less bleeding risk on dual vs triple therapy (not surprising)
– not enough evidence for comment on hard outcomes RE ischemic events
– more trials neededhttps://t.co/xtooFXtVui— Hawkins Gay, MD, MPH (@hcg_md) March 17, 2020





 © 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.
© 2025 Mashup Media, LLC, a Formedics Property. All Rights Reserved.